views
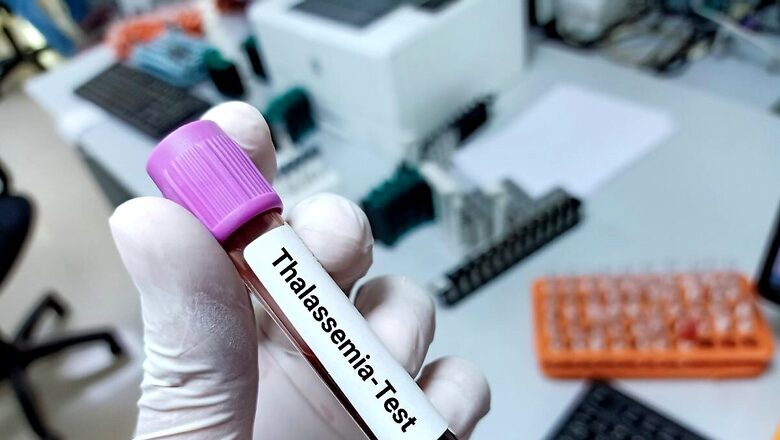
Integrate thalassemia along with the sickle cell anaemia elimination mission, the chief of the National Thalassemia Welfare Society (NTWS) has urged the government on the World Thalassemia Day on Monday.
According to government data, India has the largest number of children with Thalassemia major – nearly 1.5 lakh — and almost 4.2 crore carriers of beta thalassemia trait. Close to 15,000 babies with thalassemia major are born every year and are dependent on transfused blood for survival. Overall, there are more than 27 crore thalassemia patients in the world.
According to Dr JS Arora, general secretary of the National Thalassemia Welfare Society, “After polio, sickle cell elimination is the biggest health project of the central government. Thalassemia should not be left behind in this mission as both are genetic blood disorders.”
News18.com first reported in November about the central government’s plan to eliminate sickle cell disease from India by 2047.
The government has decided to screen 7 crore people in a mission mode for sickle cell ananemia over the next three and a half years with a focus on 17 selected states.
Sickle cell disease (SCD) is a genetic blood disorder where red blood cells contort into a sickle shape, whereas thalassemia is an inherited blood disorder characterised by less oxygen-carrying protein (haemoglobin) and fewer red blood cells in the body than normal.
Several experts have raised questions about government focusing more on sickle cell programme than thalassemia. They feel the reason could be that the former is more prevalent among the tribal community, therefore, the government has increased its focus on the well-being of their population.
NTWS has been working on the prevention of thalassemia since 1991. It stimulated all thalassemia associations of India to come on a common platform and created the Federation of Indian Thalassemics where all societies can interact and work for the common cause at the national level.
Easy to screen thalassemia with SCD
Arora, who is also a member of the ethics committee at the Indian Institute of Technology (IIT), Delhi, explained that the procedure of screening for sickle cell disease is almost similar to screening for thalassemia.
“Screening of sickle cell anaemia is done by using a solubility test. This approach saves money but will miss a few cases of sickle beta-thalassemia.”
He suggested that the addition of a simple blood test called complete blood count (CBC) can serve the dual purpose of identifying other hemoglobinopathies along with sickle cell anaemia without adding human resources.
“This can be initiated at least in 17 states targeted under the sickle cell mission…”
Status of Patients in India
The National Blood Transfusion Council has made the availability of blood free of cost for Thalassemics. However, Arora highlighted that thalassemics require “leukodepleted packed red blood cells” for transfusion.
Leukoreduction consists of eliminating leukocytes in all blood products below the established safety levels for any patient type.
Leukocytes are the cause of certain adverse reactions associated with blood transfusion.
“Only very few blood banks provide leukodepleted blood.”
While many states have started providing iron chelators — to remove excess iron from blood transfusions in the body — free of cost at transfusion centres, it’s not available at all centers across India.
“Also, due to the government’s e-Marketplace (GeM) portal, the procurement agency has to purchase from sellers having the lowest price (L-1) amongst the available sellers on the GeM. Thus quality is compromised.”
Arora highlighted that many patients, in fact, are complaining about increased side effects and/or in-effectiveness of these free medicines provided by the government.
“In that case, some patients pay out of pocket to purchase quality medicines and many consume half-heartedly without much benefit or stop it due to side effects. The government should focus on quality also not just on cost,” he suggested.
Also, he added, many patients who are highly iron overloaded or have developed complications need two or even three chelating agents. “At most of the centres only one chelator is available. This leads to inadequate treatment resulting in serious iron overload damaging vital organs causing early death.”
He recommended that all three chelators of good quality be made available at all thalassemia day care centres and each district must have at least one well-equipped comprehensive thalassemia daycare centre.
Is new treatment around the corner?
So far, there are no cures for thalassemia apart from blood transfusions for entire life.
However, stem cell transplantation (SCT) is now an established curative treatment. “There are very few transplant centres in the government sector. The government should come up with more transplant centres in public hospitals where SCT should be done free or at nominal cost.”
However, with small family norms, it’s difficult to get matched donors from within the family.
Hence, Arora suggested that there should be a public donor stem cell registry just like blood banks where volunteers can register and donate whenever the need arises. “The government grants and CSR funding can be used to make it free or at a highly subsidised cost to the recipient.”
Also, gene therapy in blood disorders like thalassemia, sickle cell anaemia and haemophilia has become a reality. “Gene insertion has already been approved for thalassemia in the USA. Gene editing, relatively a new safe technology, has also shown promising results.”
Arora urged the government to initiate research on gene therapy for hemoglobinopathies in India, which will be a boon for those who don’t have matched identical donors available.
How can the disease be prevented?
NTWS and many other thalassemia NGOs are putting their all efforts to create awareness in the public. However, their resources are limited. “The government should create awareness about the disease at war footing to sensitize the public as it has taken for HIV and polio,” said Arora.
Thalassemia awareness and screening can be linked with “Anemia Mukt Bharat”, he suggested.
Secondly, thalassemia screening in pregnant women during the first trimester should be made mandatory, he added.
“By saving one thalassemia birth we will be saving around 2,000 units of blood and over Rs 1 crore during his/her lifetime.”
He further suggested that every state should have at least one (bigger states 2-3) pre-natal diagnostic labs for hemoglobinopathies.
Read all the Latest India News and Karnataka Elections 2023 updates here


















Comments
0 comment