
views
Making Beneficial Lifestyle Changes

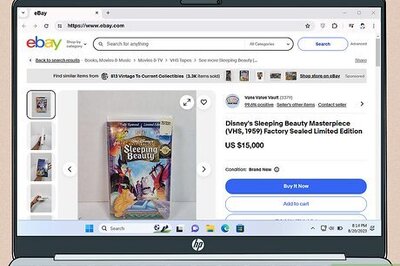
Avoid taking supplements and antacids that contain calcium. If your blood calcium levels are high, your doctor will likely instruct you to limit the amount of calcium you consume. The first step is to stop taking any supplements, antacids, or other over-the-counter products that contain calcium. If you take a daily multivitamin, ask your doctor to recommend one that doesn’t contain calcium. If you have an upset stomach, take a medication that doesn’t contain calcium, such as bismuth subsalicylate (better known as brand names like Pepto-Bismol and Kaopectate). Just be sure to check the ingredients, as some bismuth subsalicylate products contain added calcium. Check prescription medications you’re taking as well. Thiazide diuretics for blood pressure and lithium carbonate therapy could increase your calcium levels.Warning: Even if you’re in perfect health, taking too many calcium supplements or antacids can cause serious medical issues. Always use any supplement or medication as directed.
Drink at least 8 to 10 cups (1.9 to 2.4 L) of fluids per day to prevent kidney stones. Kidney stones form from built-up calcium in your body. Increase the amount of water you drink, and avoid or limit your consumption of beverages that contain calcium, such as milk. Drinking 8 to 10 cups (1.9 to 2.4 L) of fluids per day is a good general recommendation, but follow your healthcare provider’s specific advice. Check your urine to make sure you’re staying hydrated. It should be light in color. If it’s dark yellow, you need to drink more fluids. Never wait to drink until you’re thirsty, as thirst indicates that you’re already in the first stages of dehydration.
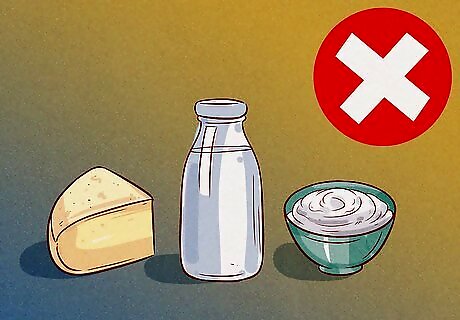
Eat fewer calcium-rich foods if your doctor advises. You may need to limit calcium in your diet or avoid it altogether, at least in the short term. Dairy products are richest in calcium so, with your doctor’s guidance, limit or avoid items such as milk, cheese, and yogurt. Limit yourself to less than 1,000 mg of calcium every day. Other sources of calcium include leafy greens and calcium-fortified cereals and non-dairy milks. For most people, calcium is an important part of a healthy diet, so check with your doctor before making dietary changes.
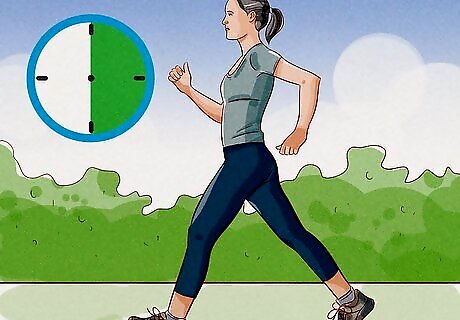
Exercise for 30 minutes a day or as much as possible. Sometimes, hypercalcemia is associated with low activity levels. If you’re able to, try to get at least 30 minutes of low- to moderate-intensity exercise per day. Good ways to keep active include walking briskly, climbing stairs, and bike riding. Check with your doctor before starting a new exercise routine if you’re not used to physical activity, especially if you have a medical condition. If you have a medical issue that restricts your mobility, ask your healthcare provider for tips about staying active despite your condition.
Identifying the Underlying Cause
Tell your doctor about your diet, family history, and symptoms. High calcium levels are usually diagnosed through routine blood tests. If your test results are abnormal, talk to your doctor about your diet and any supplements or medications you take. Let them know if you’ve experienced any unusual symptoms and if anyone in your family has a history of hypercalcemia, parathyroid issues, or cancer.Symptoms of Hypercalcemia: While most people don’t experience symptoms, signs of hypercalcemia include nausea, vomiting, loss of appetite, increased thirst, muscle weakness, bone pain, fragile bones, fatigue, and confusion.
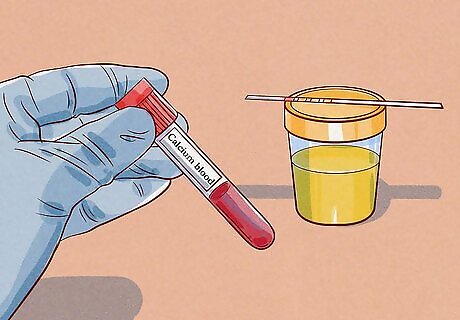
Ask your doctor for calcium blood and urine tests. Calcium levels are typically tested during a routine blood test called a basic metabolic panel. If your initial test results were abnormal, your doctor may order another calcium blood test, as well as a urine test, to confirm the results. Since it’s related to calcium absorption, your doctor may also order a vitamin D blood test. These tests are non-invasive, so there’s no need to be nervous. They’re no different than the blood and urine tests you’d receive at a routine check-up. Robert Thompson Robert Thompson, Endocrinologist For chronic hypercalcemia, addressing the root cause is essential yet complex, often requiring repeat testing and trial-and-error with medications. Quick fixes like aggressive IV fluids can help acute spikes but worsen long-term calcium metabolism. Have patience, stick to the game plan, and communicate openly with your care team. With diligence to find the perfect treatment regimen, even stubborn high calcium levels can normalize.
Get a parathyroid hormone (PTH) blood test. If your calcium levels are high, your doctor will most likely order a PTH test to check your parathyroid function. The test simply involves taking a blood sample and, usually, there’s no need to fast or otherwise prepare in advance. The parathyroid glands are tiny, located in the neck, and help regulate vitamin and mineral levels in the blood. About 90% of chronic hypercalcemia cases are caused by hyperparathyroidism, or overactive parathyroid glands.
Undergo imaging tests as recommended by your doctor. If your PTH count is high, your doctor may order a specialized imaging test to see if any of the 4 parathyroid glands are enlarged. Alternatively, if your PTH count is normal or low, they may order tests to look for certain cancers, such as lung and breast cancer. High calcium levels related to cancer are uncommon, so try not to worry. If your levels are high, you should be able to manage the condition with lifestyle changes, routine check-ups, and medication.
Managing High Calcium with Medical Treatment

Seek immediate medical attention if you have severe, acute symptoms. Excessively high calcium levels can hurt the kidneys, brain, and heart. Treatment for acute hypercalcemia typically includes IV (intravenous) fluids and diuretics, which are medications that increase urination. You may also need dialysis if elevated calcium in your blood has caused kidney failure. Sudden, severe hypercalcemia may be caused by an underlying medical condition or by consuming too many calcium supplements or antacids. Symptoms may include vomiting, diarrhea, abdominal pain, dizziness, poor balance, and confusion. These symptoms can be associated with a variety of medical issues, so see your doctor for an accurate diagnosis.
See your doctor for routine check-ups if your condition is mild. For many people, managing chronic hypercalcemia involves making lifestyle changes and monitoring blood calcium levels. If your levels are only slightly elevated and you don’t experience symptoms, your doctor will probably just recommend regular blood work. Your doctor will let you know how often you need to get your calcium levels tested. You may need to schedule check-ups every 3 to 6 months.
Take a prescription medication that controls calcium levels as directed. For moderate or severe hypercalcemia, you may need to take short or long-term medication. The right medication depends on your specific symptoms and condition. Be sure to take any medication exactly as prescribed. To manage calcium levels and prevent bone loss, your doctor may prescribe calcitonin. Spray in 1 nostril daily, and alternate spraying it in your left and right nostrils. Side effects may include nausea, runny nose, and nosebleeds. If your PTH count is high, your doctor may prescribe a calcimimetic, such as cinacalcet It’s typically taken with food once a day around the same time every day. Side effects may include upset stomach, dizziness, and weakness. If you have hypercalcemia related to cancer, your specialist may prescribe a bisphosphonate. These medications are available as tablets or monthly IV drips. Side effects may include nausea, heartburn, and flu-like symptoms. Your doctor may also use IV fluids for hydration and volume expansion.
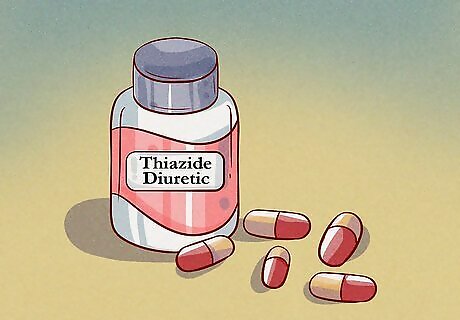
Switch your diuretic or blood pressure medicines, if necessary. If you take a thiazide diuretic or blood pressure medication, your doctor will switch you to a non-thiazide alternative. Other medications, such as lithium, can also lead to hypercalcemia, so tell your doctor about any over-the-counter or prescription drugs you take.Warning: Don’t stop taking a prescription medication without first consulting your prescriber.
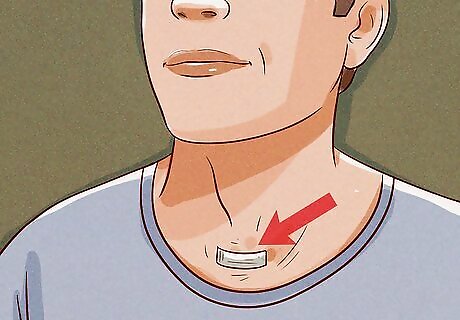
Treat serious symptoms related to hyperparathyroidism with surgery. Usually, only 1 of the 4 parathyroid glands is affected, and the operation is typically minimally invasive. While you may stay overnight, many patients are able to go home the same day of surgery. You’ll have a sore throat for a few days and should stick to liquid and semi-solid foods. Most patients take prescription pain medication for 2 to 3 days after the operation. Depending on the extent of surgery, you should be able to resume normal activities in less than a week. You’ll usually be recommended surgery if you have calcium higher than the upper normal limit greater than 1, osteoporosis, vertebral fracture, chronic kidney disease, high urinary calcium, kidney, stones, or if you’re over 50 years old.

















Comments
0 comment