
views
X
Trustworthy Source
PubMed Central
Journal archive from the U.S. National Institutes of Health
Go to source
This transition period usually passes within 4-6 weeks, and in the meantime, you can ease your discomfort with remedies like aloe and ice, improve your retinol usage technique, and take other skin-healthy measures. That said, make sure to see your doctor if you show signs of an allergic reaction or a serious “retinol burn.”
Treating Painful Skin Symptoms

Apply ice to inflamed spots to temporarily reduce your discomfort. Wrap a bag of ice or an ice pack in a clean, soft towel and hold it to the problem area for up to 15 minutes per hour. Icing the area will provide some short-term pain relief, but won’t do anything about the redness or peeling. Never apply a bag of ice, an ice pack, or an ice cube directly to your skin. You run the risk of causing skin damage or even frostbite. Also, if your skin is already peeling, the ice may stick to it and cause it to tear away when you remove the ice.

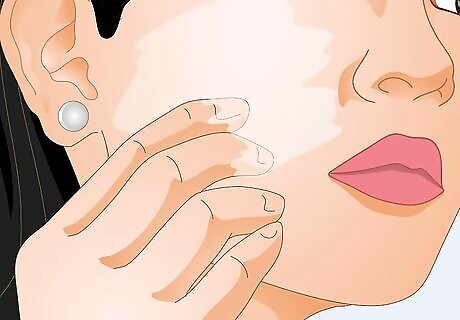
Use aloe vera or 1% hydrocortisone on dry or peeling patches of skin. Try adding small dabs of 100% aloe vera gel to problem areas as often as needed throughout the day. If aloe doesn’t help, try using OTC 1% hydrocortisone gel. Follow the package instructions regarding application amount and frequency, or consult your doctor for directions. Hydrocortisone may help ease your skin’s inflammatory response to the retinol. It turns out that retinol activates the same “irritant receptor” as capsaicin, the key component of pepper spray.

Consult your doctor if you get cracked, oozing skin or significant discomfort. Most cases of “retinol burn” consist of redness, irritation, dryness, and/or peeling. If your skin gets dry and irritated enough that it cracks and either oozes or bleeds, stop using the retinol product and call your primary care doctor or dermatologist. Do the same if you experience anything beyond mild-to-moderate pain. Your doctor may advise using a less potent concentration of retinol and/or cutting back on how often you use it. For some people with sensitive skin, though, retinol simply isn’t a good option.
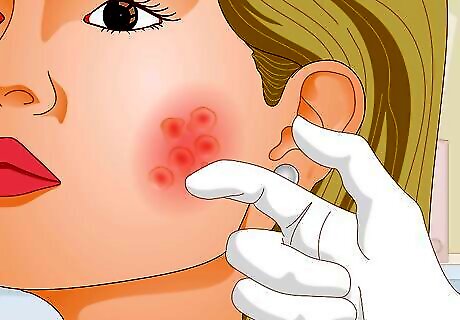
Seek medical attention if you have signs of an allergic reaction. While uncommon, an allergic reaction to retinol can be a serious problem. If you develop hives or swelling in the application area, and especially if they’re rapid-onset, stop using the product and get in touch with your doctor as soon as possible. If you experience difficulty breathing or swallowing, get emergency medical assistance right away. If you have experience dealing with allergies, follow the treatment plan—such as applying hydrocortisone or taking an antihistamine—that tends to work for you. If you carry an EpiPen due to your risk of serious allergic reactions, use it if needed and contact emergency services. Try taking diphenhydramine (Benadryl) immediately if you’re experiencing a mild allergic reaction.
Changing How You Use Retinol

Try an OTC retinol if a prescription product is causing you problems. There is a wide range of both OTC and prescription retinol products on the market, and OTC options typically have lower retinol concentrations. If you started with prescription retinol and have experienced a lot of discomfort, ask your doctor about switching to a lower-concentration OTC product. Even if you did start with an OTC product, you may be able to switch to one with a lower concentration. Ask your primary care doctor or dermatologist for product recommendations.
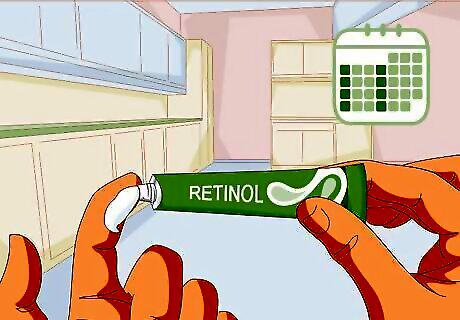
Cut back to using retinol twice per week, then slowly increase the frequency. If you started off using retinol once per day or even once every other day, try cutting back to twice or even once per week. Slowly increase the frequency over time as your skin becomes sensitized to the retinol. Try the following plan: Use retinol twice per week (one application each day) for 2 weeks. Move up to 3 times per week for 2 weeks, and keep adding a day every 2 weeks. Slow down the process further so that you’re adding a day every 4 weeks if necessary.
Apply retinol at night in a small amount to clean, fully-dry skin. A little retinol goes a long way, so a pea-sized dab is plenty for your entire face. Unless your primary care doctor or dermatologist advises otherwise, try the following routine: Wash the treatment area—most commonly your face—about 40-60 minutes before bedtime and rinse it thoroughly with cool water. Gently pat the area dry with a soft towel, then let it air dry for 20 minutes. Work a small amount of the product into your fingers, then gently massage it over your treatment area. Let the product dry for about 20 minutes before going to bed.Tip: Always apply topical retinol at night since sunlight can make it less effective.

Use a gentle, basic moisturizer either before or after using retinol. Opinions differ on the best way to incorporate moisturizer into a retinol routine. Experts do agree that, if you do use a moisturizer, you should choose a gentle, basic one without fragrances or unnecessary ingredients. Talk to your dermatologist or primary care doctor about the best way to utilize moisturizer along with retinol. While some experts advise against using both retinol and moisturizer, most experts are pro-moisturizer and fall into one of the following categories: Apply retinol, let it dry, then apply moisturizer. Apply retinol immediately before applying moisturizer. Apply moisturizer, let it dry, then apply retinol. Apply moisturizer immediately before applying retinol.
Making Additional Skincare Adjustments
Use a gentle skin cleanser on any areas where you apply retinol. If you’re applying retinol to your face—by far the most common spot—use a gentle face cleanser such as Cetaphil or similar brands. Use the cleanser twice per day—in the morning and in the evening before applying retinol. The gentler you are when cleaning your skin, the less irritated it’s likely to become from using retinol. Your doctor may recommend a prescription skin cleanser in some cases.

Stop using any exfoliants, scrubs, or masks. Even if you regularly used one or more of these before starting retinol, stop any and all of them immediately. Remember that the goal is to be as gentle as possible to your skin while using retinol. It’s possible that, after your skin has adjusted to the retinol—which usually takes around 4-6 weeks—you might be able to start using these types of products again. However, you’ll likely see such positive results from the retinol that you won’t have any reason to use them. Avoid using any harsh soaps, detergents, or cosmetics until the burned area heals.

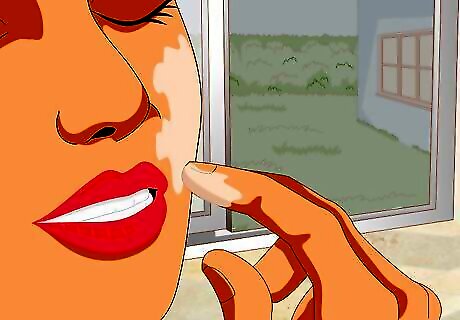
Wear a gentle but effective sunscreen every time you go outdoors. Retinol makes your skin much more sensitive to the sun’s rays, so it’s critical that you wear sunscreen, even on cloudy days. As with your moisturizer, choose a sunscreen that is gentle, basic, and without non-essential ingredients. Ask your primary care doctor or dermatologist for recommendations. Even when wearing sunscreen, you may want to limit your exposure to the sun’s rays, especially around mid-day, at least for your first 4-6 weeks on retinol.

Hydrate your skin by drinking enough water. Despite the unproven claims you may find online, drinking lots of water doesn’t magically cure dry skin. However, consuming a healthy amount of water each day will keep your entire body—including your skin—better hydrated. Everyone’s hydration needs vary due to a range of factors, but you almost certainly aren’t getting enough water if you frequently feel thirsty. The old notion that you should aim to drink 8 glasses—or 64 fl oz (1.9 L)—of water per day is no longer supported by medical science. If you want a set daily water goal, talk to your doctor so you can determine one based on your particular circumstances. Try drinking a half-glass or full glass of water when you wake up and go to bed, as well as before meals. Take sips of water throughout the day, before you feel thirsty.
















Comments
0 comment