
views
X
Trustworthy Source
Cleveland Clinic
Educational website from one of the world's leading hospitals
Go to source
Inform any sexual partners about the diagnosis, practice safe sex for the rest of your sexual life, and abstain from sex while treating genital warts or during any future outbreaks.
Applying Medicated Ointment
Get a prescription medication from your doctor. Don’t use over the counter medications intended for warts in other locations. Have your doctor or dermatologist examine the affected area. For external warts, they’ll likely prescribe a medicated ointment. External warts affect the skin’s surface. Your doctor will recommend cryotherapy — a procedure in which the warts are frozen off using liquid nitrogen. They may recommend another method if warts affect areas that aren’t suitable for ointment, such as mucous membranes, the urethra, or inside of the vagina. Additionally, surgical removal might be your best option if large areas of skin are affected or if you have some medical conditions, such as an immune disorder.
Have your doctor show you how to properly apply medication. There are a few kinds of ointment available, and each has a different application method. Ask your doctor to demonstrate proper application techniques. Make sure you clearly understand the instructions before leaving the office. It's important that your doctor shows you exactly how to apply medication. Improper application can worsen side effects, such as irritated skin, or render the treatment ineffective. The three types of medicated ointments or gels are imiquimod, podofilox, and sinecatechins. Follow the specific instructions for the medication your doctor prescribes. Ask your doctor how long you'll need to apply the ointments for them to be effective.
Wash your hands before and after applying ointment. Wash up with soap and hot water for 20 seconds, then dry your hands thoroughly. Make sure they’re completely dry before you handle the ointment or gel. Be sure to wash your hands again after applying medication. Medications for genital warts can irritate skin, so it’s important to make sure you wash away any excess from your hands. Furthermore, touching other surfaces after treating warts could spread germs.
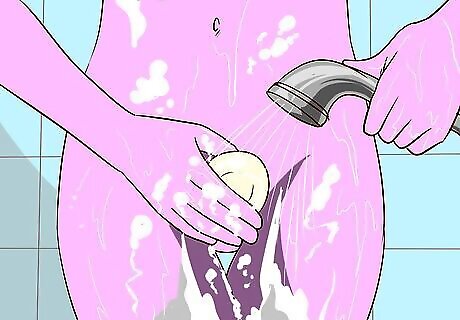
Wash and dry the area to be treated before applying medication. Take a shower or just the wash the affected area. Clean it with soap and hot water, then dry the area thoroughly. The area needs to be completely dry before you apply medication.
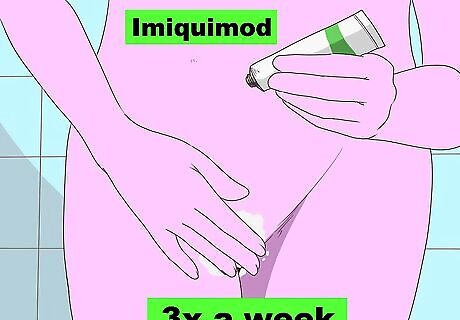
Apply imiquimod at bedtime, then wash the area after 6 to 10 hours. If you’re prescribed imiquimod, use your finger to apply a thin coating to the wart or warts. Wash the area with soap and warm water 6 to 10 hours after applying the ointment. The number of times you’ll apply imiquimod depends on its strength, so ask your doctor how often you should use it. Apply a higher strength ointment before bed 3 times per week. Apply a lower strength dose every night before bed. You’ll need to wash the area 6 to 10 hours after application regardless of the dosage strength.
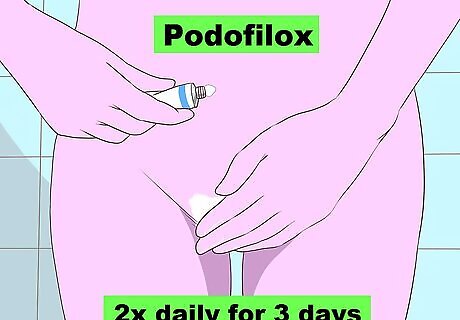
Apply podofilox twice daily for 3 days if your doctor prescribed it. Podofilox is available as a solution, which you apply with a cotton swab, and a gel, which you apply with your finger. Apply just enough medication to lightly coat each wart twice a day 3 days in a row. After 3 days of using podofilox, don’t apply any medication for 4 days, then repeat the 3 application day cycle. Complete up to 4 cycles of 3 days of application and 4 days of no application. Ask your doctor if you should wash the treated area after several hours. Remember that your doctor will only prescribe one type of topical medication. Follow the instructions to apply podofilox only if your doctor prescribed it.

Apply sinecatechins 3 times a day if your doctor prescribed it. Use your finger to lightly coat each wart with sinecatechins. Use it 3 times a day for up to 16 weeks, or according to your doctor's instructions. Don't wash the area after applying sinecatechins. Keep in mind you'll only apply one type of medicated ointment. If your doctor prescribed sinecatechins, you won't need to use podofilox or imiquimod. Your doctor may prescribe you one treatment and then have you switch to a different treatment later on.
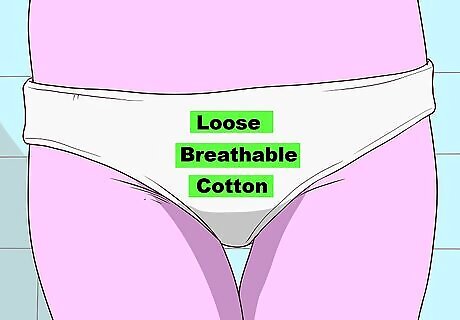
Cover the area only with breathable cotton. Wear loose, breathable cotton underwear after applying an ointment or gel. It’s not necessary to bandage the area, but it might be more comfortable to do so if the spot is prone to rubbing against surrounding skin or your underwear. If you want to cover it, use cotton gauze only, and don’t use a waterproof bandage. If you use a dressing, change it at least twice a day or after bathing. You can also wear a pad or panty liner and change it out throughout the day.
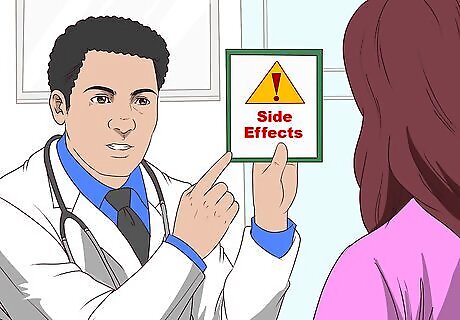
Talk to your doctor if you experience side effects. Common side effects of any medicated ointments prescribed for genital warts include redness, burning, and pain on the application side. If any of these are severe, ask your doctor if you should use a different medication or one at a lower concentration.
Having Warts Chemically or Surgically Removed
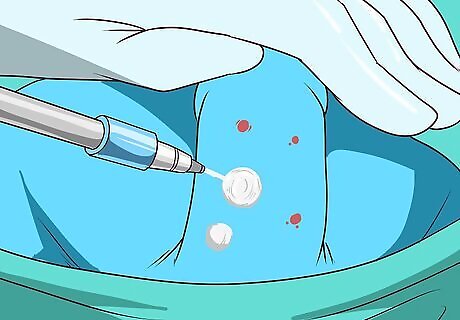
Have urethral or cervical warts surgically removed during your visit. If warts affect a spot that’s not suitable for medicated ointment, or if the area is too widespread for ointments or gels, your doctor will recommend chemical or surgical removal. Options include cryotherapy, — when the warts are removed by freezing — laser removal, and surgical removal by incision. Your doctor will most likely administer a local anesthetic, so you probably won't feel anything at all during the procedure. You might experience some minor pain and swelling after, but it will go away in a few days. You may feel discomfort with laser removal, but not pain. If you saw a specialist, such as a dermatologist, urologist, or gynecologist, they'll likely remove the warts during your initial visit. If you saw your primary doctor, they might not have experience performing a procedure or the right equipment. If necessary, they'll refer you to a specialist. You can also visit a local STD clinic to have your genital warts removed.
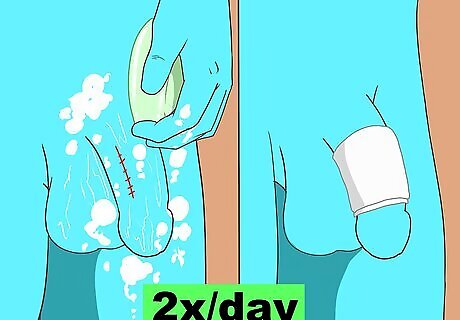
Wash the surgical site twice daily and dress it with a bandage. After having your procedure, follow your doctor’s care instructions. They’ll likely advise you to wash the area with soap and warm water 2 times per day. After washing the area, dress it with a clean, dry bandage. Remember to wash your hands before and after caring for and dressing the affected area.
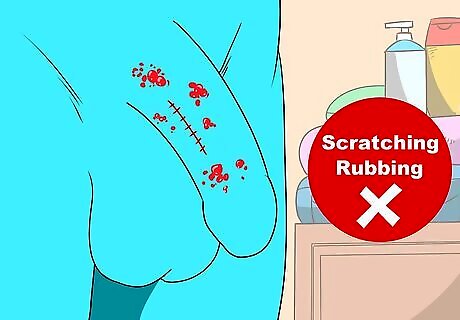
Avoid scratching or rubbing any blisters that develop. After cryotherapy, it’s common for blisters to form over the treated site. It’s important to leave them alone, so don’t scratch or try to pop them. They’ll go away on their own after several days. In rare cases, blisters or the incision site can become infected. Call your doctor if redness or swelling worsen after 24 to 48 hours, or if you notice pus or discharge.

Discuss interferon therapy if other methods are unsuccessful. If all other methods are unsuccessful, some doctors recommend injecting interferon, or an antiviral medication, into the affected area. Side effects include flu-like symptoms, such as fever, muscle aches, chills, and pain at the injection site. Depending on the type of injection, you’ll have to see your doctor for treatments 2 to 3 times a week for 3 to 8 weeks.
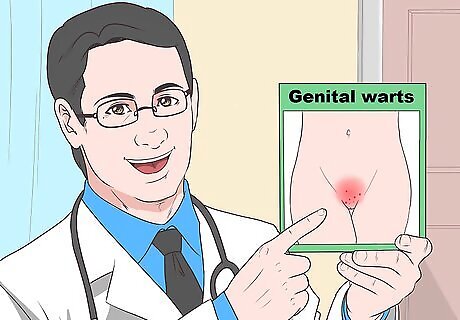
Managing HPV
Don't feel ashamed or think you did something wrong. HPV is incredibly common, so don't be hard on yourself. In the United States, about 80 percent of sexually active people will contract HPV at some time in their lives. Most people don't develop any symptoms, and it often goes away on its own. Diagnosing HPV in males is more difficult because they often don't show any symptoms. When you're considering a new sexual partner, make sure you both get tested at an STD clinic. Scientists don't completely understand how the virus goes dormant, but in most cases, a healthy immune system can suppress HPV within 1 to 2 years.
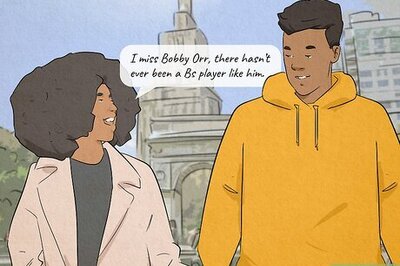
Inform any sexual partners if you have genital warts. If you’re diagnosed with HPV, you should tell your past or current sexual partners. There’s no way to tell when you might have contracted HPV; warts can develop weeks, months, or years after the initial exposure. Treating an outbreak will not cure HPV, so you should inform future partners as well. Ask your doctor for information about the specific strain of HPV you contracted. There are well over 100 strains, and there are very few cases of strains that can cause reproductive cancers. Ask your doctor if you're at risk of developing a reproductive cancer. It's a tough conversation to have, but try to be direct and honest. Tell past partners, "I want to let you know that I recently received treatment for HPV. It's impossible to know when or how I contracted it, but I thought you'd want to know and get tested." You don't have to share every detail of your sexual history with a new partner, but you should allow them to make an informed decision before having sex, especially if you've ever received treatment.

Avoid sexual contact during an outbreak or when treating warts. It's easier to spread the virus that causes genital warts during an outbreak. Additionally, the treated area will be irritated, so you'll need to avoid sexual contact. Ask your doctor how long you should wait before having intercourse after treatment. The length of time you should avoid intercourse depends on the type of treatment you receive. Treating warts reduces but doesn’t completely eliminate, the risk of spreading HPV.

Wear a condom during sex even when no warts are present. Using condoms will help reduce the risk of spreading HPV. However, even if you use a condom, there’s still a risk of spreading the virus through skin contact. Areas of the skin that aren’t covered by a condom can be affected by genital warts and spread the HPV virus.
See your doctor if you have another outbreak. After initially treating genital warts, it’s common to experience another outbreak within 3 months. If necessary, schedule a follow up appointment with your doctor for a second round of treatment.

















Comments
0 comment